An Andrological Update: The ‘small’ world of Andrology
Stuart Dawe-Long, Andrology Lead/Training Lead (Senior Clinical Scientist), Manchester University NHS Foundation Trust
Welcome! No, you have not read the title incorrectly and I do realise that this blog is for the British Association of Cytology (BAC), but there are some Cytologists that do andrology activities! Regardless, I hope you find this interesting.
Introduction
Manchester University NHS Foundation Trust is home to the Department of Reproductive Medicine. The Andrology service provides Manchester, Greater Manchester and beyond with accredited diagnostic services, long-term storage of gametes prior to treatment, supports the embryology service in preparation of samples for treatment and houses the UK National External Quality Assessment Service (UK NEQAS) for Reproductive Science scheme. We currently have capacity to analyse approximately 4000 samples for diagnostics and approximately 700 ‘new’ long term storage referrals per year. The team really does rely on each one of us, which includes:
- Clinical Scientists
- Biomedical Scientists
- Advanced Associate Practitioners
- Associate Practitioners
- Biomedical Support Workers
- Scientific Training Programme (STP) students
What is Andrology?
Generally, most services will consider semen analysis as the role of an Andrology department. This is, in fairness, probably true for most. Those who may not know we undertake the following diagnostic tests:
Post vasectomy semen analysis (PVSA): we analyse semen to assess if sperm remain present after a vasectomy. Where sperm are detected, we need to quantify numbers (as a concentration) and the movement of the sperm (motility).
Diagnostic Semen Analysis (DSA): semen is examined both macroscopically and microscopically. The following parameters are assessed:
- Volume (mL)
- pH
- Colour, viscosity and liquefaction
- Concentration and total sperm number per ejaculate (x106/mL and x106/ejaculate)
- Motility (% into four categories)
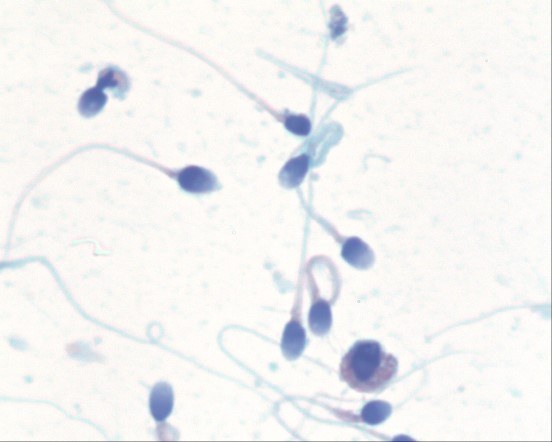
- Morphology (% normal forms), see Figure 1.
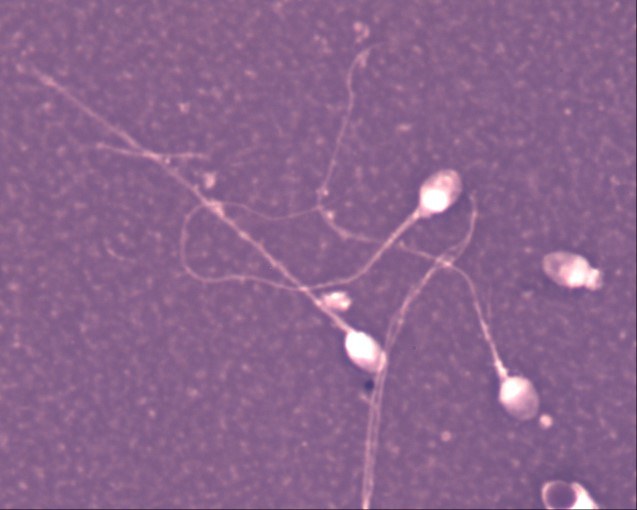
- Vitality (% viable or ‘living’ sperm), see Figure 2.
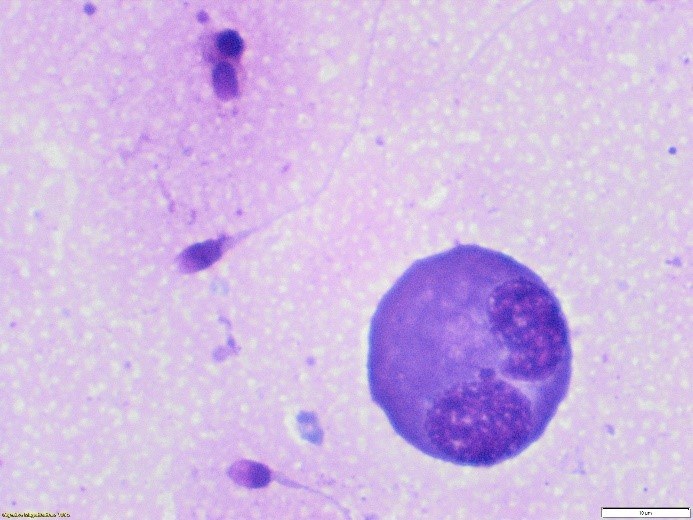
- Non-sperm cells (x106/mL), see Figure 3.
Retrograde ejaculation: this test involves analysing post-orgasm urine for the presence of sperm. This can be supported with methods of neutralising urine to support sperm motility if the sample is required for storage or treatment.
Services may also provide other services including storage, testing samples for treatment options, preparation of samples for treatment or advanced diagnostics. Regardless, most Andrology departments will have patient contact beyond most other life science areas! Something that can be challenging but ultimately one of the most rewarding parts of our job. This gives us an opportunity to listen to the patient and have the privilege of being part of their journey.
Long Term Storage (LTS)
This is one of the key activities within our service at Manchester, where we provide LTS under the Human Fertilisation and Embryology Authority (HFEA) licenced activities. Here, our senior team undertake consultation clinics for patients that may be referred to store gametes prior to:
- Chemotherapy for cancer treatment
- Surgery that may impact sexual function and/or the production of sperm
- Hormonal treatment for patients (such as people who are transgender)
- Stem cell transplants (for sickle cell patients)
The team will support the patient to understand the consent forms required to obtain informed consent and explain the implications of their decisions. Alongside this, we support the person holistically, providing them with an opportunity to ask questions and signpost them if necessary to other services such as counselling. The laboratory team will then process their sample, undertaking a semen analysis and protecting the sample from too much damage as they slowly freeze the sample (controlled rate freezing). Small ampules are then stored in liquid nitrogen, in the vapour phase at approximately -196 degrees Celsius in large storage tanks (Figure 4).

The future of Andrology?
Andrology is now recognised as a discipline in its own right! In 2018 The Academy for Healthcare Science (AHCS) launched an equivalent route for Biomedical Scientists to apply and allow registration as a Clinical Scientist with the Health and Care Professions Council (HCPC). Students on the Scientific Training programme (STP) can choose Andrology as their main discipline, which has now created the opportunity for application on the Higher Specialist Scientist Training (HSST) programme to work towards a doctorate level qualification (DClinSci). I am currently on this programme as the first Andrology intake (wish me luck)! In addition to this, I have been working with the Institute of Biomedical Science (IBMS) and other Andrology experienced scientists (shout out to Emma Whitehouse at Good Hope Hospital) to create a Specialist Diploma in Andrology, covering seven core modules:
- General Andrology Laboratory Procedures
- Fundamentals in Male Infertility
- Diagnostic Semen Analysis
- Reporting of Diagnostic Semen Analysis
- Retrograde Ejaculation
- Post Vasectomy Semen Analysis
- Quality Management
These are due for release in October 2024!
Hopefully, the development of training and qualifications in Andrology will support Consultant Andrology roles within healthcare and provide improvements in patient pathways and align with the NHS Long Term Workforce Plan. I have previously supported the management of patients for sexual dysfunctions, such as erectile dysfunction and undertaken male infertility review clinics, which has included examination of the patient, organising tests (such as USS) and providing advice – something I would be keen to bring into reproductive medicine in the future as the role develops. Hopefully, as we are more integrated into the healthcare science workforce we can review how we may support patients and current staff safely and effectively.
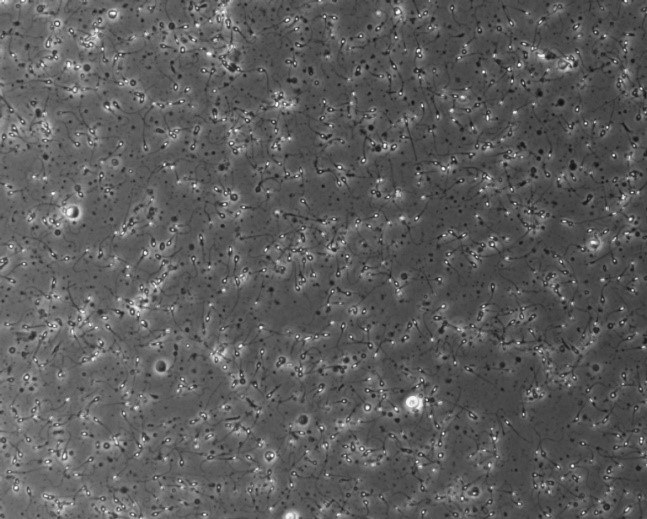
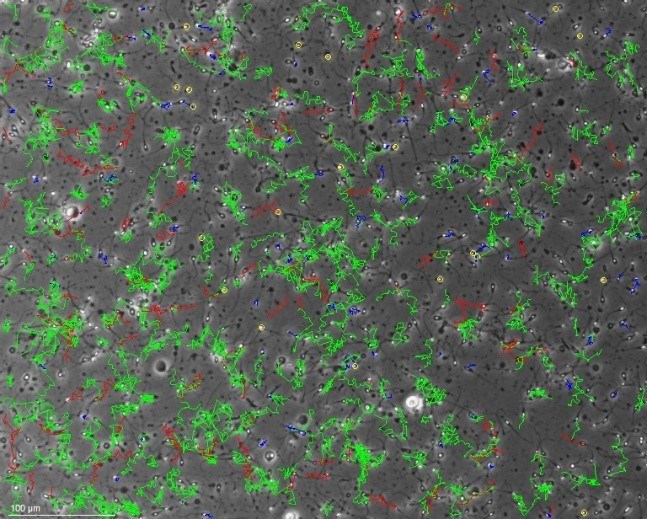
Scientifically, Andrology has scope to progress. Many centres are implementing computer assisted semen analysis (CASA). Figure 5a demonstrates a routine motility view using phase contrast microscopy and Figure 5b demonstrates the image using CASA. These can be used to create personalised reports and support analysis capacity within busy services.
There are also some services that have implemented advanced diagnostic tests for patients, such as sperm DNA fragmentation testing (sDF) for breaks in the DNA, oxidative stress/reactive oxygen species testing and assessment of acrosome reaction (the acrosome reaction is required for oocyte penetration to take place).
Here in Manchester, we are also training our Andrologists to support the surgical sperm retrieval (SSR) pathway from start to finish. Scientists attend a Consultant Urological Andrology Surgeon at theatre to retrieve samples for processing. This may be from testicular tissue or from epididymal aspirations. During attendance we must adhere to aseptic techniques, follow good operating department practice and assure accuracy of collection activities. These are then transported by incubation to the Embryology clean rooms where the team prepare samples under microscopy for identification of sperm and cryopreservation if these are detected. This is a joint effort between Embryology and Andrology and one which showcases the developing roles we have as scientists!
Conclusion
Whilst many Andrology services provide patients with diagnostics, there are many others that specialise in this area and cross clinical boundaries. There are many opportunities for scientists to develop and exciting possibilities that expand out of the ‘bench in the corner’ we once were. Hopefully, more people can be encouraged to go into this exciting career and really burst out of the small world we were once considered.
