Current dilemmas and future solutions in cervical screening
Karen Kendall Cytology Service Lead Royal Wolverhampton NHS Trust (RWT). Louise Etchells Cytology Operations Manager/Deputy Manager
Karen and Louise provide an excellent update and valuable insight into the current dilemmas and future solutions facing cervical screening in the UK

Karen Kendall Cytology Service Lead Royal Wolverhampton NHS Trust (RWT). Louise Etchells Cytology Operations Manager/Deputy Manager
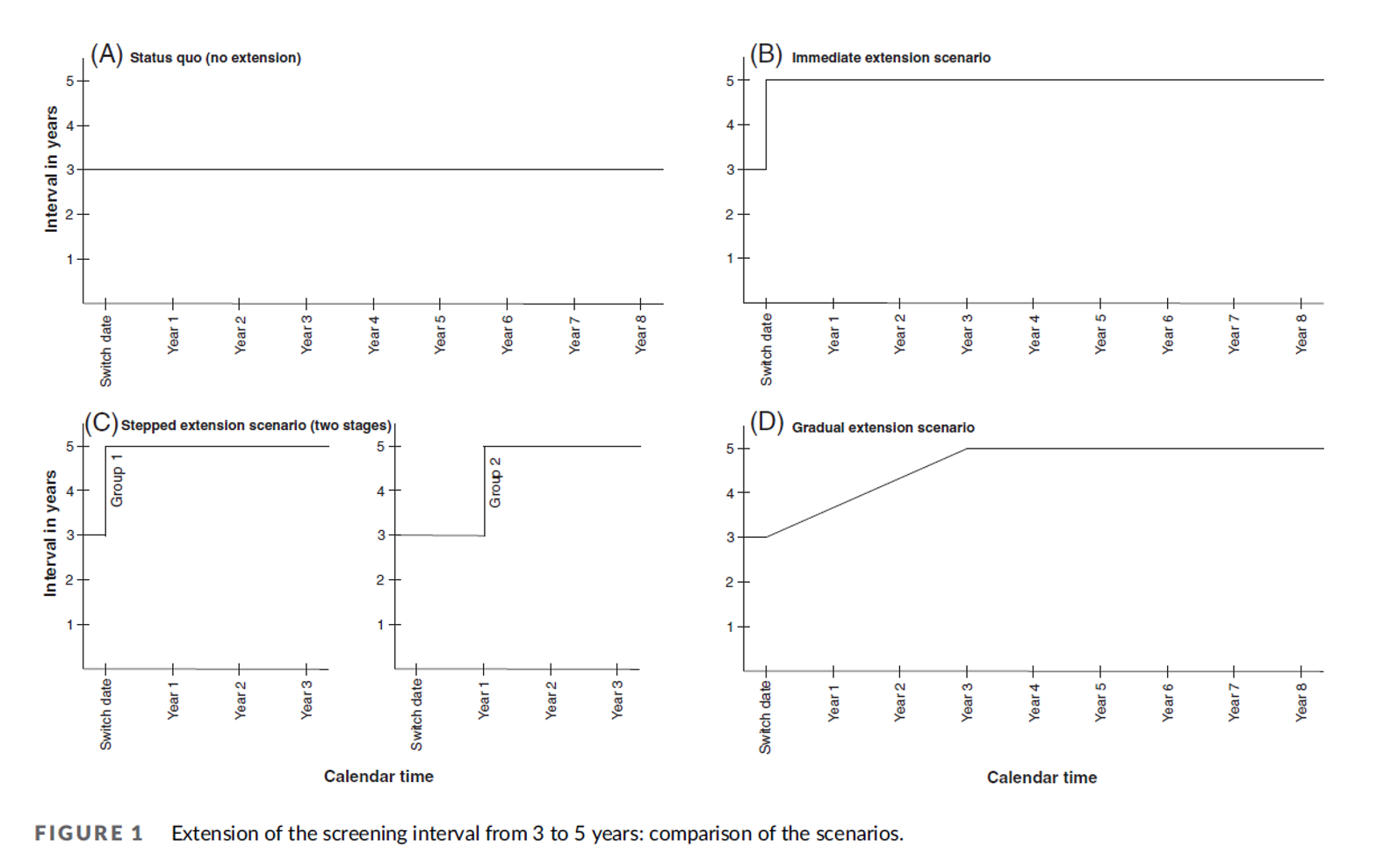
All 8 English cervical cytology screening laboratories have been granted a two-year extension for the cytology service which expires in May 2026. This reflects the expected ‘go live’ date for the new Cervical Screening Management System (CSMS) which replaces the existing Open Exeter system. We are also waiting in anticipation for the extended recall of negative HPV test reports from three years to five years and although the service is uncertain how this will be implemented it may well have a significant impact on the workforce in screening laboratories. The method used could set peaks and troughs for the whole screening programme. Journals suggest that an immediate interval extension from 3 years to 5 years could lead to a difference in workflow estimated to be up to 4-fold which will re occur cyclically for several screening rounds. If subgroups were determined within the extended interval the peaks and troughs would be flattened, (ref: Francesca Pesola 2022) this will enable streaming of work force planning.
HPV vaccinated cohorts are coming into the screening programme in substantial numbers, it is likely that there will be a significant drop in cytology numbers. This will exacerbate the existing problem of screeners unable to reach a 3000 per annum target set by the NHSCSP. Wales have addressed this by setting a Welsh standard of 1000 per annum. Ref: Gareth Powell: (Public Health Wales – Screening, SCW Llantrisant). The laboratory clinical professional group (CPG) for the English programme set up a working group some time ago to review the 3000 target which was based on the primary cytology programme. To date no outcome to reflect the current HRHPV Cytology service from this group been agreed upon.
As the screening service is constantly being reviewed the future may involve a further consolidation of services which will in turn exacerbate the problem of recruitment to all roles. By way of future proofing the service RWT is engaging with a pilot scheme to trial Consultant Cytopathologists working from home. This may be extended to all screening grades in the future.
The department recognises that homeworking can bring advantages both to the employee and to the department and partner trusts. These include flexibility around issues such as reduced costs, better use of time, convenience, freedom from transport problems and ecological benefits.
It is NHS policy to introduce more flexible ways of working and, in the context of networks, approaches to service provision and access to digital systems, working at home may provide part of a solution for some aspects of the service. Initiatives in the NHS are linked to developing seven days working, and flexible use of staff resources will be required.
The department anticipates that with the adoption of digital microscopy, opportunities to deliver a cytological diagnostic service from home will present themselves.
To align with the proposition of digital microscopy, our department is also participating in a pilot scheme to evaluate the Hologic Genius system; participating laboratories will have to make adaptations to their current staining protocols in order to incorporate the Hologic imager stain and film coverslips; these changes are currently being undertaken and validated.
Due to time constraints, two digital systems are being placed in the Halo Laboratory London and the Royal Derby Hospital. It is hoped that initial study data will be available to be presented to the UK National Screening Committee in December 2023. More extensive study data will then be obtained by placing evaluation systems in further sites in the future to embellish the initial feasibility and workflow data.
This will have a huge impact on the future of Cytology and if implemented it could streamline screening times and potentially allow for a further merge of services as there will be a decrease in the time allocated for screening each slide which could therefore increase productivity and efficiency.
RWT has undertaken a project within the BCPS (Black Country Pathology Service), to reflect the current workforce and projected needs of the department going forward. This has highlighted an aging population of staff in more senior roles. To address this, succession planning is currently being undertaken and staff at all levels are being developed on an individual basis ensuring cover and contingency throughout the career pathway. The department has recently recruited two WTE biomedical scientists who are also undertaking training for competence in cervical cytology. Additionally, we offer Principal Advanced Practitioner posts for experienced staff interested in undertaking Consultant BMS roles in the future.
Other developments in the Cytology service may include genomic testing for the presence of High-Risk HPV or other cancer markers within non-gynaecological samples, demonstrating the need for extended roles for cytoscreeners, to include molecular processing and diagnostic cytology sample preparation.
Similarly, DNA methylation levels correlate with cytologic and histologic grades, especially CADM1 in women with HPV types 16 and 18, and this supports the concept of using genomic DNA methylation as a molecular modifier in cervical screening. (Ref: Wiyada Dankai 2019).
Trials are currently being conducted in self-sampling for cervical screening but results have not as yet been published. The studies aim to validate the self-sample device/test combination for sensitivity and specificity and allow insight into the logistics of processing self-testing and associated costs as well as assessing the acceptability to the user of the self-testing method and creating a database to be used in future technology development and evaluation. People who are HPV positive would need a clinician taken sample to allow for any subsequent cytology screening. The main aim of self-sampling is to increase the uptake of cervical screening in women as coverage continues to fall year on year.
Staff involved in the cervical screening programme have become used to adapting to the changing service requirements. This is set to continue; the current requirements are likely to change in the coming years with potentially more involvement in molecular technologies along with the use of digital and home reporting. Staff may find their roles develop to incorporate a mix of skills making their work potentially more varied and fulfilling.
References:
1. PMID: 30608989 PMCID: PMC6319776
Managing an extension of screening intervals: Avoiding boom and bust in health care workloads.
Pesola F, Rebolj M, Sasieni P. Int J Cancer. 2023;152(10):2061‐2068. doi:10.1002/ijc.34441 2068 PESOLA ET AL.
2. 2019 Jan 4;14(1):e0210289. doi: 10.1371/journal.pone.0210289. eCollection 2019
Role of genomic DNA methylation in detection of cytologic and histologic abnormalities in high risk HPV-infected women.
Wiyada Dankai 1 2, Surapan Khunamornpong 1 2, Sumalee Siriaunkgul 1 2, Aungsumalee Soongkhaw 1, Arphawan Janpanao 1, Utaiwan Utaipat 3, Nakarin Kitkumthorn 4, Apiwat Mutirangura 5, Jatupol Srisomboon 1 6, Suree Lekawanvijit 1 2
